The Definitive Guide to Cognitive Behavioral Therapy CPT Codes
Table of Contents
Here is a hard truth: Mental health practices lose an estimated 10-15% of their annual revenue simply because of coding errors.
Imagine performing a high-intensity trauma session, doing the heavy lifting of cognitive restructuring, and then getting paid for a standard check-in because you swapped a 90837 for a 90834. Or worse, facing a clawback audit two years later because your documentation didn’t support the “Interactive Complexity” add-on you routinely use.
If you are a therapist, biller, or practice manager, you know that clinical excellence and revenue cycle management are two different beasts. You might save lives in the therapy room, but if you can’t translate that work into the correct cognitive behavioral therapy CPT code, your practice’s financial health will suffer.
This guide isn’t just a list of numbers; it’s a strategic playbook. We are cutting through the jargon to give you the exact codes, time rules, and billing nuances you need to get paid what you are worth.
Key Takeaways: The “Cheat Sheet” Strategy
- Time is Money: The difference between 90834 and 90837 is strictly time-based. Missing the 53-minute mark by one minute forces a downcode.
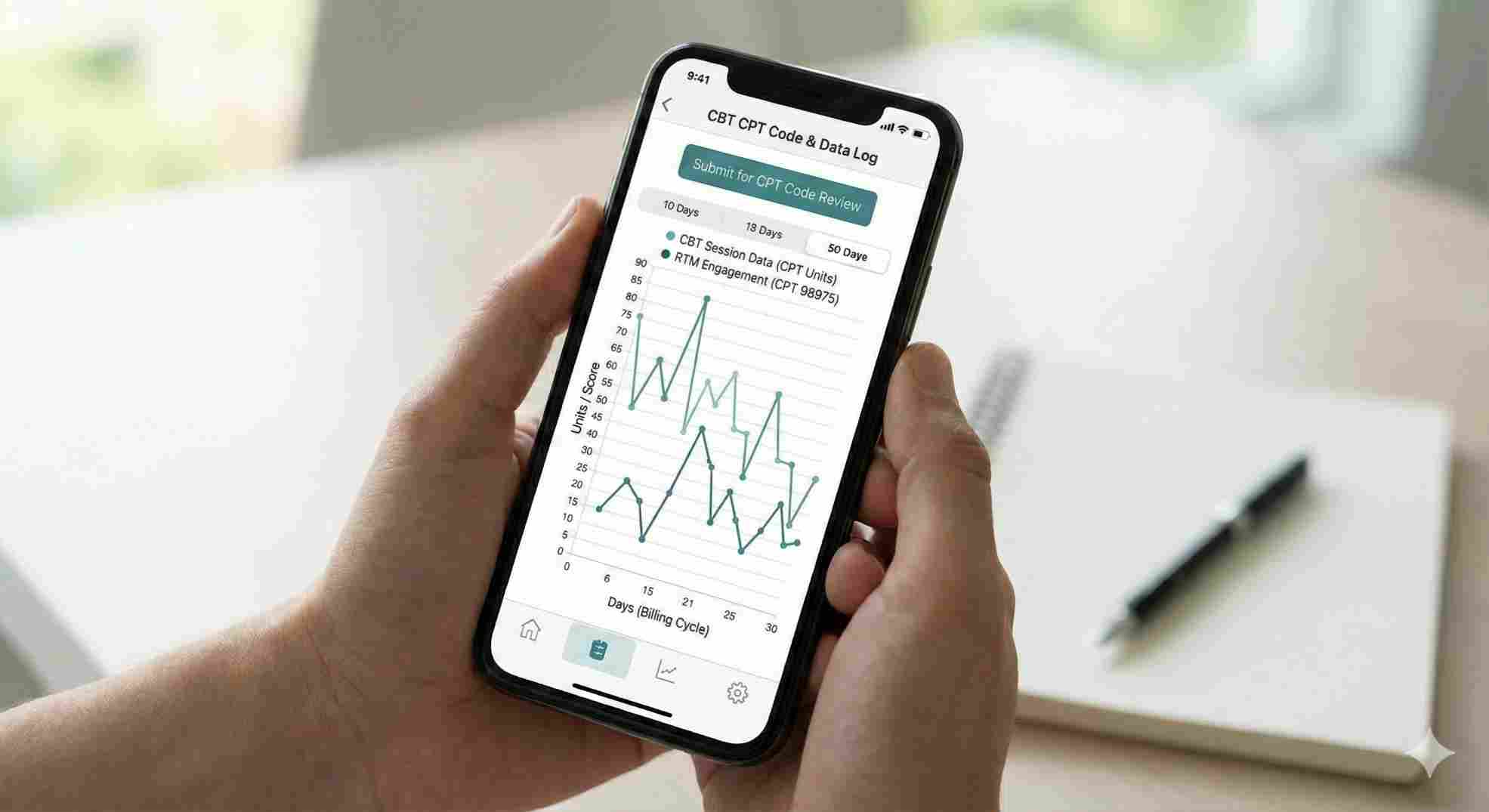
- Digital is Here: New Remote Therapeutic Monitoring (RTM) codes (like 98978) allow you to bill for asynchronous CBT data collection.
- Add-Ons are Critical: Crisis codes and interactive complexity codes (+90785) can significantly boost reimbursement for difficult sessions.
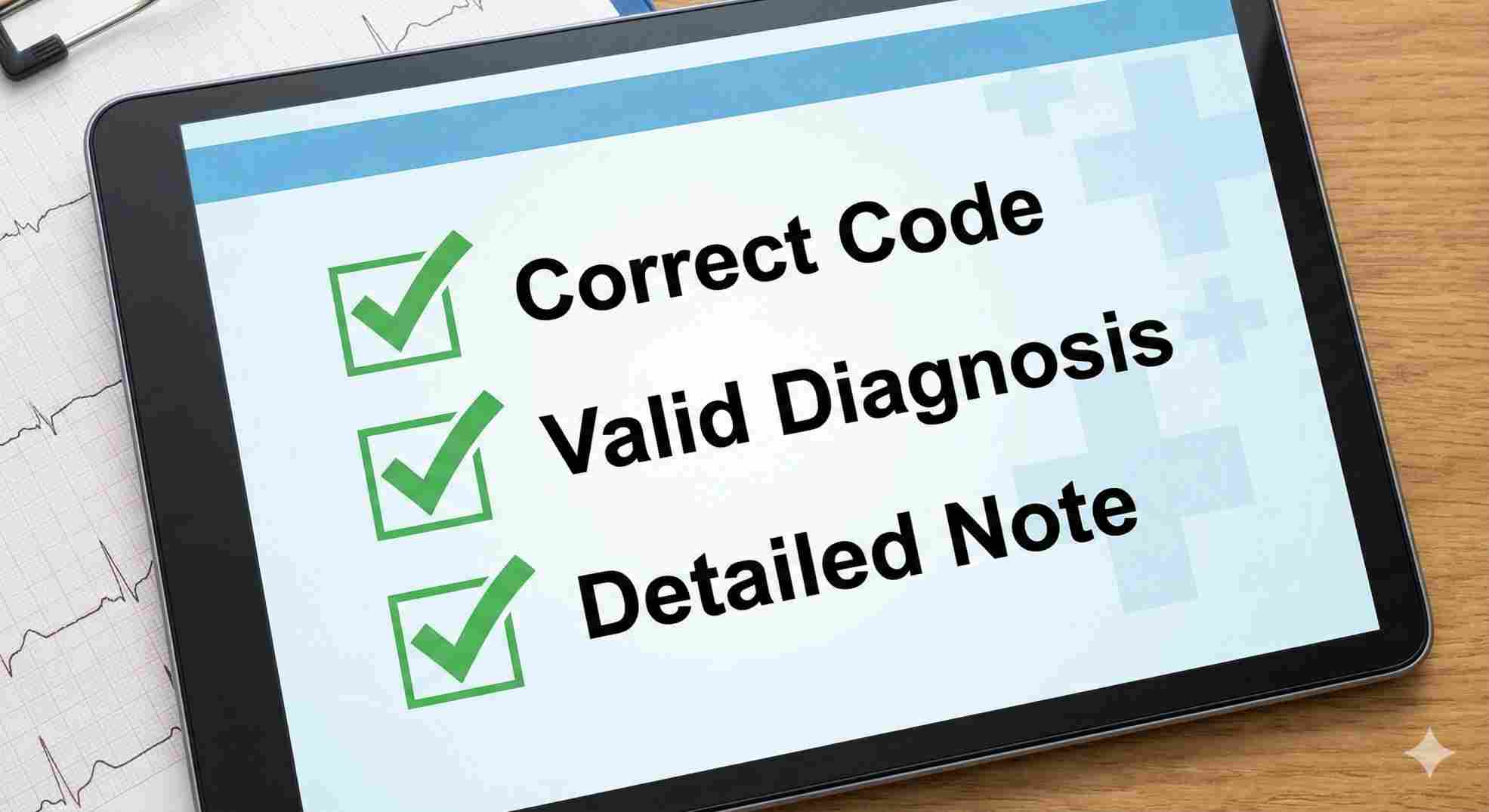
- Documentation: “Patient tolerated session well” is not enough. You must document specific interventions (e.g., “Socratic questioning,” “exposure hierarchy”).
The Core Cognitive Behavioral Therapy CPT Codes
Let’s clear up a common misconception: There is no single “CBT CPT code.”
CPT (Current Procedural Terminology) codes are procedure-based, not modality-based. According to the American Medical Association (AMA), whether you are doing CBT, DBT, or ACT, you bill based on time and setting. However, the way you document CBT specifically justifies these time-based codes.
Here are the three heavy hitters you will use 90% of the time.
90832, 90834, and 90837: The Time Rules
Insurance auditors love these codes because they are easy to verify. If your note says “Session time: 45 minutes” but you bill 90837, you are non-compliant.
| CPT Code | Description | Required Duration | Typical Reimbursement (Medicare Avg) |
|---|---|---|---|
| 90832 | Psychotherapy, 30 minutes | 16–37 minutes | ~$79 |
| 90834 | Psychotherapy, 45 minutes | 38–52 minutes | ~$104 |
| 90837 | Psychotherapy, 60 minutes | 53+ minutes | ~$154 |
The “Aha!” Insight: Many therapists fear billing 90837 (the 60-minute code) because they believe it triggers audits. This is largely a myth if you actually spend 53+ minutes face-to-face. If you do a standard 50-minute clinical hour, you must bill 90834. To bill 90837, you need to extend that session past the 53-minute mark.

Documentation for CBT Validity
To support these codes, your notes must reflect CBT-specific interventions as outlined in best practices by the American Psychological Association (APA).
- Weak: “Discussed anxiety.”
- Strong: “Utilized cognitive restructuring to challenge catastrophic thinking regarding work performance. Assigned thought log for homework.”
Crisis and Complexity: When Sessions Go Off-Script
CBT often involves exposure therapy or trauma processing, which can lead to highly emotional, unpredictable sessions. Standard codes don’t cover the extra intensity or time.
Crisis Codes: 90839 & +90840
Use these when a patient is in high distress and requires immediate attention that interrupts your schedule. This is not for a scheduled session that happens to be emotional.
- 90839: First 60 minutes of crisis psychotherapy (requires urgent assessment/history of a crisis state).
- +90840: Each additional 30 minutes.
Interactive Complexity: +90785
This is an “add-on” code. You use it on top of your standard interview or therapy code (like 90791 or 90834).
Use this when:
- Maladaptive communication interferes with the session.
- Caregiver emotions interfere with the treatment (common in CBT with children).
- You must report a sentinel event to a third party (like CPS).
Note: You cannot simply add this because the session was “hard.” You must document specific factors like “high reactivity” or “use of play equipment for communication.”
The New Frontier: Digital CBT and RTM Codes
This is where the industry is heading. In 2025 and 2026, payers are increasingly recognizing Remote Therapeutic Monitoring (RTM). Recent updates from CMS.gov Physician Fee Schedule indicate that if you assign digital CBT homework via an app or platform, you might be eligible for these codes.
| CPT Code | Purpose | Service Description |
|---|---|---|
| 98978 | Device Supply | Supply of device for cognitive behavioral therapy monitoring (billable once every 30 days). |
| 98980 | Treatment Mgmt | First 20 minutes of RTM treatment management services per month. |
| 98981 | Add-on Mgmt | Each additional 20 minutes of RTM treatment management. |
Why this matters: These codes acknowledge that CBT happens between sessions. If you review patient data from a CBT app (like mood logs or exposure trackers) and spend 20 minutes a month doing it, you can get paid for that time.
Group and Family CBT Codes
CBT isn’t always a solo journey. Group CBT (for anxiety, depression, or substance use) is highly effective and efficient for your practice revenue.
The Distinction: Patient Present vs. Absent
- 90853 (Group Psychotherapy): This is for general group CBT. Reimbursement is per person. If you run a group of 8, you bill this code 8 times.
- 90847 (Family/Conjoint Therapy): The patient is present. You are working on family dynamics using CBT principles.
- 90846 (Family Therapy w/o Patient): The patient is not present. Example: Teaching parents how to reinforce a child’s exposure exercises.
Common Billing Pitfalls to Avoid
Even with the right cognitive behavioral therapy CPT code, you can get denied. Here is how to bulletproof your claims.
1. The “Modality” Confusion
Do not look for a code that says “CBT for Insomnia” or “CBT for OCD.” You will not find one (except for very specific RTM device codes). You bill the psychotherapy code (90834) and link it to the diagnosis code (ICD-10, e.g., F42.2 for OCD).
2. Modifier Mayhem
- Modifier 95: Essential for Telehealth sessions.
- Modifier 25: Used by psychiatrists/prescribers doing medication management (E/M code) AND therapy (add-on code like +90833) in the same visit. It tells the insurer, “These were two distinct services.”
3. The “Medical Necessity” Trap
Auditors look for progress. If you bill 90837 for 50 sessions with the exact same note (“Patient stable, continued CBT”), you are a target. CBT is goal-oriented. Your notes must show:
- Progress toward a goal.
- A change in the treatment plan if progress stalls.
- Specific homework assigned and reviewed.
Conclusion: Stop Guessing, Start Strategizing
Mastering the cognitive behavioral therapy CPT code landscape isn’t about memorizing 8,000 numbers. It’s about knowing the core five or six codes that drive your revenue and understanding the rules that govern them.
Don’t let poor coding undermine your clinical success. Audit your last 10 notes today. Did you bill 90834 but only write for 35 minutes? Did you miss an interactive complexity add-on?
Ready to optimize your practice’s revenue cycle? Start by implementing the time-tracking protocols we discussed above, and ensure your documentation explicitly states the “CBT interventions” used. Your bottom line will thank you.
FAQs About the cognitive behavioral therapy cpt code
Can I bill 90837 and 90834 on the same day?
Is there a specific CPT code for CBT-I (Insomnia)?
How do I bill for scoring a CBT assessment (like the BDI or PHQ-9)?
Does Medicare cover the RTM code 98978?
What if my session lasts exactly 37 minutes?
Schedule Zoom Meeting
Ready to stop leaving money on the table? Navigating the complexities of CPT codes and RTM updates shouldn’t take time away from your patients. If you want to ensure your practice is fully compliant and maximizing every reimbursement opportunity, it is time to bring in the experts. Explore our
Ready to stop leaving money on the table? Navigating the complexities of CPT codes and RTM updates shouldn’t take time away from your patients. If you want to ensure your practice is fully compliant and maximizing every reimbursement opportunity, it is time to bring in the experts. Explore our full range of solutions to streamline your revenue cycle today. Schedule an Appointment for
Mental Health Billing Services to streamline your revenue cycle today.

