
Master Mental Health Billing Training: The Guide to Getting Paid
Table of Contents
Are you tired of seeing “Claim Denied” stamps on the work you put your heart into? It is a sinking feeling that many private practice owners and administrative staff know too well. As we often discuss at RCM Finder, the root cause is frequently a lack of proper mental health billing training. Whether you are a solo therapist trying to wear every hat or a billing manager looking to sharpen your team’s skills, the gap between providing care and getting paid for it is widening every year.
The insurance game has changed. It used to be simple, but now, payers are looking for any reason to keep their money. If you don’t know the exact difference between a 90834 and a 90837, or if you mess up a modifier, you are working for free. It’s not just annoying paperwork; it’s the difference between a practice that thrives and one that goes broke.
This guide isn’t going to bore you with textbook definitions. We are going to talk about how to actually fix your cash flow. We’ll look at what you need to learn, which certifications are worth the money, and the daily habits that stop denials before they happen. By the end of this, you’ll have a plan to stop fighting with insurance reps and start seeing money hit your bank account.
The “Quick Win”: The 15-Minute Audit
Before you spend a dime on a course, do this free check. Call it the 15-Minute Audit.
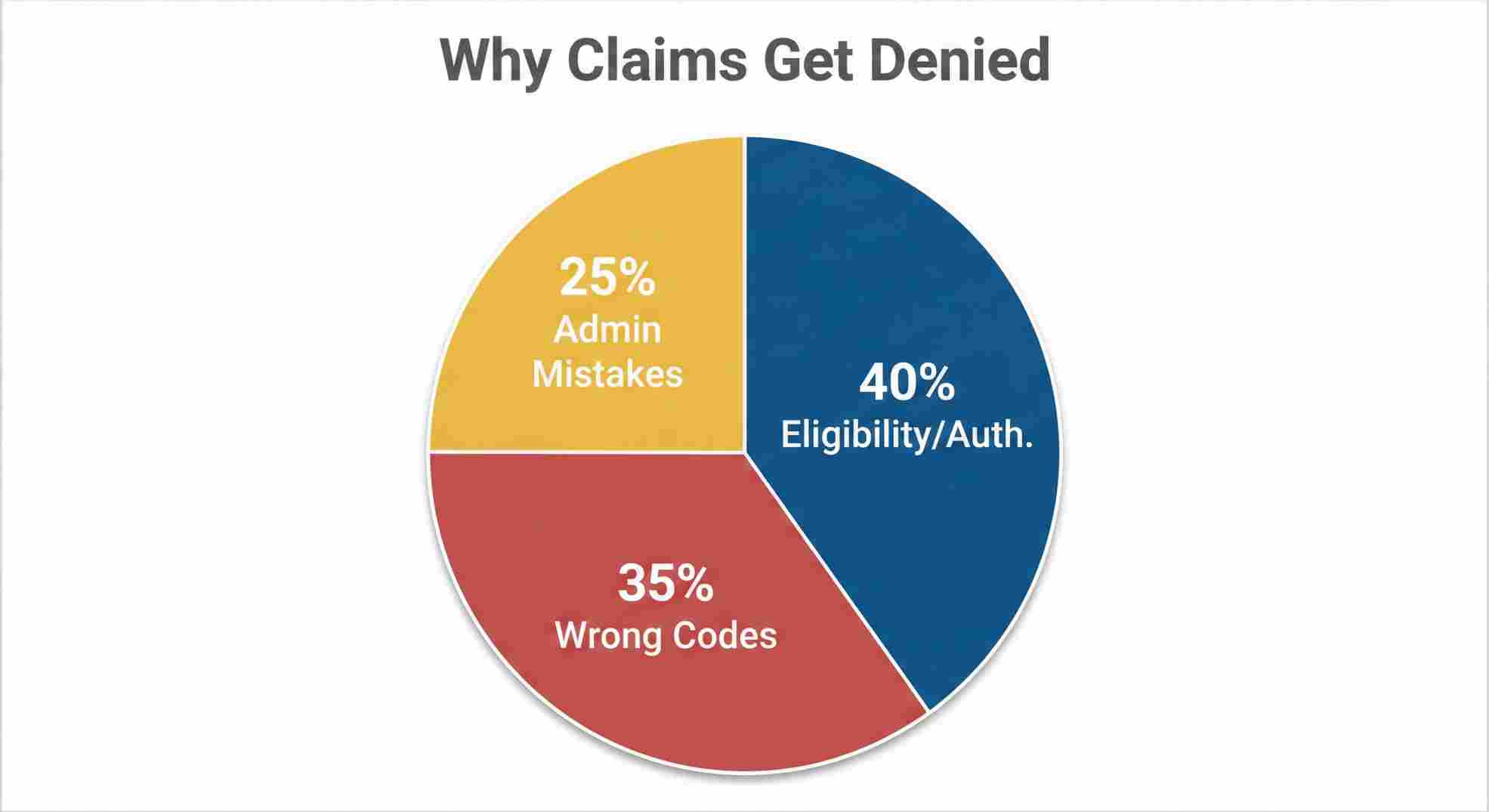
Grab your last 10 denied claims. Don’t just file them away—look at why they were kicked back. In almost every mental health practice I’ve seen, the problem comes down to three things:
- No Auth: The client’s insurance expired, or you didn’t get permission first.
- Wrong Codes: You billed for an hour (90837) but your notes only show 45 minutes (90834).
- Modifier Mess-ups: You did a video session but forgot the “GT” or “95” tag.
If you can spot which of these three traps you’re falling into, you’ve already fixed half your problem. Training isn’t always about learning new stuff; sometimes it’s just about stopping the bad habits.
Why You Can’t Just “Figure It Out” Anymore
Medical billing is hard enough, but behavioral health is its own weird world. If you break your arm, the billing is straightforward. The arm is broken, here’s the x-ray, pay me.
Mental health isn’t like that. It’s subjective. And without solid mental health billing training, you are basically guessing. When you guess, the insurance company wins.
Behavioral Health is Different
You’ll see courses for behavioral health billing training and others for mental health. They are mostly the same, but behavioral health is broader—it includes addiction and substance use.
The tricky part is that your billing has to match your time exactly. If you talk to a family member without the patient in the room, that’s a specific code. If the patient is there, it’s a different code. Generic medical billing classes skip this stuff. They teach you how to bill for flu shots, not for family therapy. If you use those generic rules, you might get paid now, but you could get audited later. And yes, they will ask for the money back.
The Real Cost of Being Untrained
Think about this: Every time a claim gets denied, it costs about $25 in staff time to fix it and resubmit it. If you see 40 patients a week and mess up 10% of the claims, you aren’t just losing the fee. You are paying thousands of dollars a year just to fix your own mistakes.
Table 1: What Ignorance Costs You
| Metric | DIY / No Training | Trained Biller | What It Means |
|---|---|---|---|
| Claims Paid First Try | 70% – 85% | 95% – 99% | Money in the bank faster |
| Time to Fix Denials | 30+ Days | 3-5 Days | Less stress |
| Cost to Collect | 8-10% of income | 3-5% of income | You keep more profit |
| Audit Worry | High (Lots of errors) | Low (Clean notes) | You sleep better |
What You Actually Need to Learn
If you are looking at a course or writing a cheat sheet for your front desk, these are the must-haves. If a program doesn’t cover these, skip it.
1. The Front Door (Intake)
Most billing errors happen before the client sits on the couch. Your training has to focus on the first phone call. You need a script. You need to verify benefits immediately. Does the client have a deductible? Is mental health managed by a different company than their medical health? Find this out on Day 1, not after 5 sessions.
2. The “Big 5” Codes
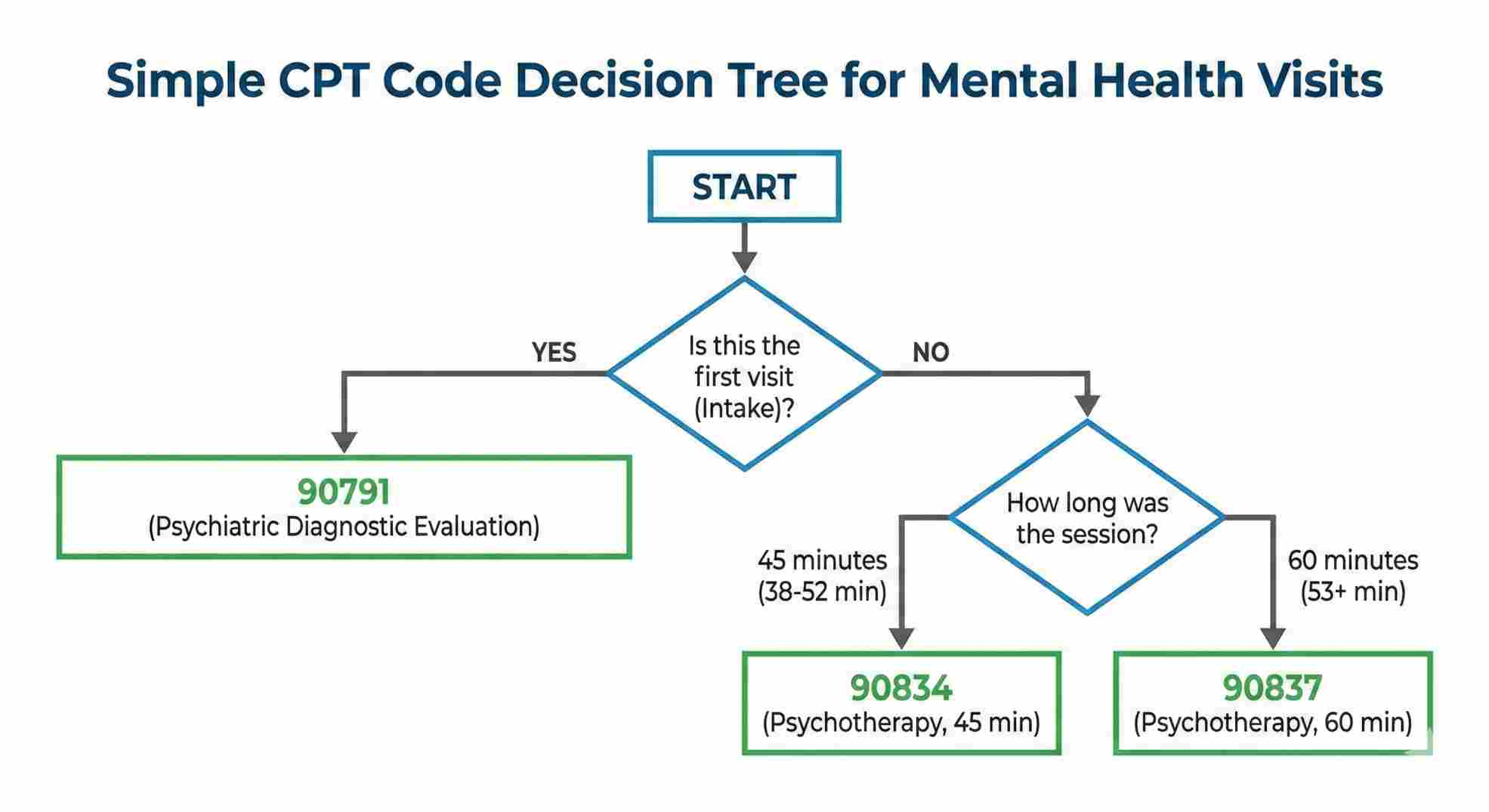
You cannot survive without knowing your codes. Your training should focus heavily on the official CPT codes defined by the American Medical Association. You need to know these “Big 5” cold:
- 90791: The intake session.
- 90834: Therapy, 45 minutes (the most common one).
- 90837: Therapy, 60 minutes.
- 90847: Family therapy (patient is there).
- 90853: Group therapy.
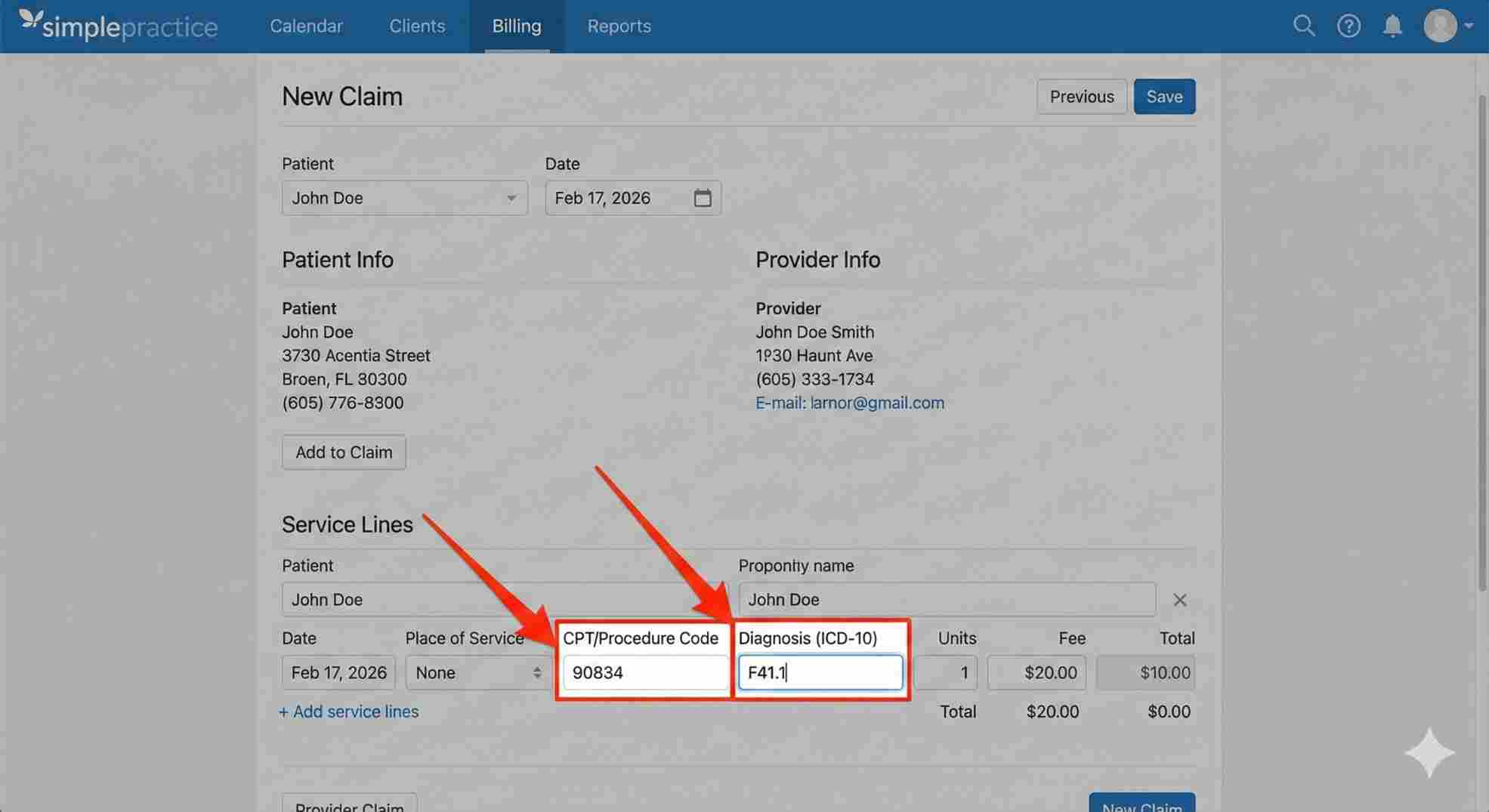
3. Diagnosis Codes (ICD-10)
You have to connect the “what” (CPT code) to the “why” (Diagnosis). A rookie mistake is using vague codes like “Unspecified Anxiety” for too long. Insurance wants specifics. Good training teaches you how to pick the right code from the DSM-5 and match it to the ICD-10 list so they can’t say it wasn’t “medically necessary.”
Best Places to Learn This Stuff
You can learn from YouTube, or you can get a serious certification. Here is who I trust.
AAPC (The Gold Standard)
These guys are the big dogs of medical coding. They have tracks for behavioral health billing training. Their “Certified Professional Biller” (CPB) badge actually means something. It’s hard work, but if you put it on your resume, people listen.
AMBA (For Business Owners)
AMBA is great if you run a practice or a billing company. They focus less on the tiny coding details and more on the business side—how to get claims paid and how to run a profitable office.
Niche Platforms
Sites like TheraPlatform or specific consultant courses are often better for solo therapists. They cut out the hospital stuff you don’t need and just show you how to bill for your private practice.
Table 2: Where to Get Trained
| Provider | Who is it for? | Cost | Certification? | Focus |
|---|---|---|---|---|
| AAPC | Career Billers | $$$ | Yes (CPB) | Strict Coding Rules |
| AMBA | Practice Owners | $$ | Yes (CMRS) | Getting Paid & Business |
| Udemy / Online | Beginners | $ | No | The Basics |
| Insurance Portals | Admin Staff | Free | No | How to use their site |

The Telehealth Headache
Since 2020, everything is different. If your mental health billing training manual is from 2019, throw it in the trash. It’s useless.
Telehealth has its own rules. You need special Place of Service (POS) codes—usually “02” or “10” depending on if the patient is at home. You also need modifiers like “95”.
The catch? Every insurance company wants something different. Blue Cross might want one modifier, while United wants another. Good training teaches you how to look up these rules, because they change all the time.
Should You Do It Yourself?
This is the big question. Do you train your front desk to do this, or do you hire a pro?
Keep It In-House
If you do it yourself, you have control. You can see who owes you money every day. But, you have to keep learning. You can’t just learn it once. The codes update every January, so you have to stay on top of it.
Outsource It
Hiring a billing company gets the work off your desk. But you still need to know the basics. If you don’t understand mental health billing training at all, you won’t know if your biller is doing a good job. You need to know enough to check their work, or you might find out six months later that they haven’t been collecting your money.
Don’t Go to Jail (Fraud & Abuse)
It sounds dramatic, but it’s real. You can’t just bill whatever you want.
“Upcoding” is when you bill for 60 minutes but only saw the client for 30. That is fraud. “Unbundling” is splitting up services to get paid more. Also fraud. A solid training program will have a section on ethics. It should teach you how to write notes that justify your billing—we call this the “Golden Thread.” The intake, the plan, and the notes all have to match.
Table 3: How to Stay Out of Trouble
| Bad Move | Why People Do It | The Consequence |
|---|---|---|
| Upcoding | Wanting more money | Audits, Fines, Losing License |
| Copy/Paste Notes | Saving time | Taking money back (Clawbacks) |
| Billing No-Shows | Recouping lost time | Illegal (You can’t bill insurance for this) |
The Software Trap
You need good tools. Electronic Health Records (EHR) like SimplePractice or TherapyNotes are great because they have billing built in.
But don’t get lazy. I’ve seen therapists trust the software too much. They assume the “default” setting is right, and then find out they’ve been submitting the wrong code for months. Learn the software, but use your training to double-check it.
The Bottom Line
Billing isn’t the fun part of the job. You didn’t get into this field to fill out forms. But if you ignore it, you burn out.
You don’t need to be a genius at math, but you do need to respect the process. Whether you get a fancy certification or just take a really good workshop, the goal is the same: clarity.
When you invest in mental health billing training, you aren’t just learning data entry. You are protecting your income. You are making sure that the time you spend helping people is actually valued. So take that 15-minute audit, see where you’re losing money, and fix it. Your practice depends on it.
FAQs About Master Mental Health Billing Training
Do I need a license to bill for mental health?
How long does it take to learn?
What is the difference between coding and billing?
Can I bill for two sessions in one day?
Why do they deny for "Medical Necessity"?
Schedule Zoom Meeting
You became a physician to treat patients, not to wrestle with insurance companies. Every hour your team spends chasing denied claims or deciphering complex coding rules is an hour lost on patient care and a direct hit to your bottom line. Don’t let administrative bottlenecks stifle your facility’s growth. Our specialized Behavioral & Mental Health Billing Services are designed to cut through the red tape, reduce your denial rate, and accelerate your cash flow. reclaim your time and ensure you get paid for every service you provide.

