97035 CPT Code: The Definitive Guide for Physical Therapists
Table of Contents
The 97035 cpt code is one of the most commonly billed—and denied—modalities in physical therapy, leaving countless clinics with money on the table. It happens more often than you think. You provide excellent care, you set up the ultrasound unit, you spend the time with the patient, but when the Explanation of Benefits (EOB) comes back, the line item is denied. It is frustrating, and quite frankly, it hurts your practice’s bottom line.
This matters now more than ever because insurance payers are looking for reasons to cut costs. Whether you are dealing with physical modalities or The Real Truth About Coding and Billing for Mental Health Services, the goal is the same: get paid for what you do. Right now, payers are targeting “passive” modalities like ultrasound with aggressive audits. If your notes don’t prove exactly why that ultrasound was necessary for that specific patient on that specific day, you are working for free.
The solution isn’t to stop using ultrasound; the solution is to master the billing. In this guide, we are going to break down exactly how to document, code, and justify the 97035 cpt code so you get paid every single time.
The “Quick Win” Insight: It’s All About Attendance
Before we dig into the details, here is the single most important thing you need to know about this code: It requires constant attendance.
Unlike unattended electrical stimulation (G0283) or mechanical traction, you cannot set up the ultrasound head, walk away to check on another patient, and bill for it. The 97035 cpt code is defined as a “timed” code. This means the CMS 8-minute rule applies. If you only do ultrasound for 5 minutes, you cannot bill a unit. You need at least 8 minutes of direct, one-on-one contact to legally submit this code to a payer. Keep this rule in your pocket—it will save you from an audit nightmare later.
What is the 97035 CPT Code Description?
To bill correctly, you have to understand what the payer sees. The official 97035 cpt code description is straightforward: “Application of a modality to one or more areas; ultrasound, each 15 minutes.”
Let’s break that down into plain English.
- Modality: This is a physical agent used to produce therapeutic changes in biologic tissues.
- One or More Areas: This is tricky. Even if you treat the right shoulder and the left shoulder, you do not automatically get to bill two units unless the time justifies it.
- Each 15 Minutes: This is the kicker. This is a time-based code.
When you use the 97035 cpt code, you are telling the insurance company that you used sound waves to generate deep heat within body tissues. This heat increases blood flow, relaxes muscle spasms, and prepares the tissue for more active procedures like therapeutic exercise or manual therapy.

Phonophoresis and 97035
A common question I get from practice owners is about phonophoresis. This is where you use ultrasound to drive medication (like dexamethasone) through the skin.
There is no specific CPT code for phonophoresis. Therefore, the American Medical Association (AMA) and most payers instruct you to use the 97035 cpt code. However, you cannot bill the medication itself under this code. The medication is usually considered a supply, which might be billed separately depending on the payer, but the service itself falls under therapeutic ultrasound.
Medical Necessity: When Can You Bill It?
You cannot just slap ultrasound on every patient with back pain and expect payment. That is a red flag. To use the cpt code for therapeutic ultrasound, you need to document specific physiological goals.
Payers want to see that the ultrasound is facilitating a return to function. It should not be the only treatment; it should be a preparation for something else. Following evidence-based practice guidelines ensures your treatment plan remains defensible during an audit.
Valid Clinical Indications:
- Restricted Joint Motion: The heat helps extensibility of collagen structures.
- Muscle Spasm: Reduces spindle activity to relax the muscle.
- Pain Control: Modulates pain to allow for movement.
- Chronic Inflammation: Helps increase blood flow to stagnant areas.
If your documentation says “Patient tolerated treatment well,” you are failing. Your notes must say why you did it. For example: “Ultrasound applied to R supraspinatus tendon to increase tissue temperature and extensibility prior to manual stretching.”
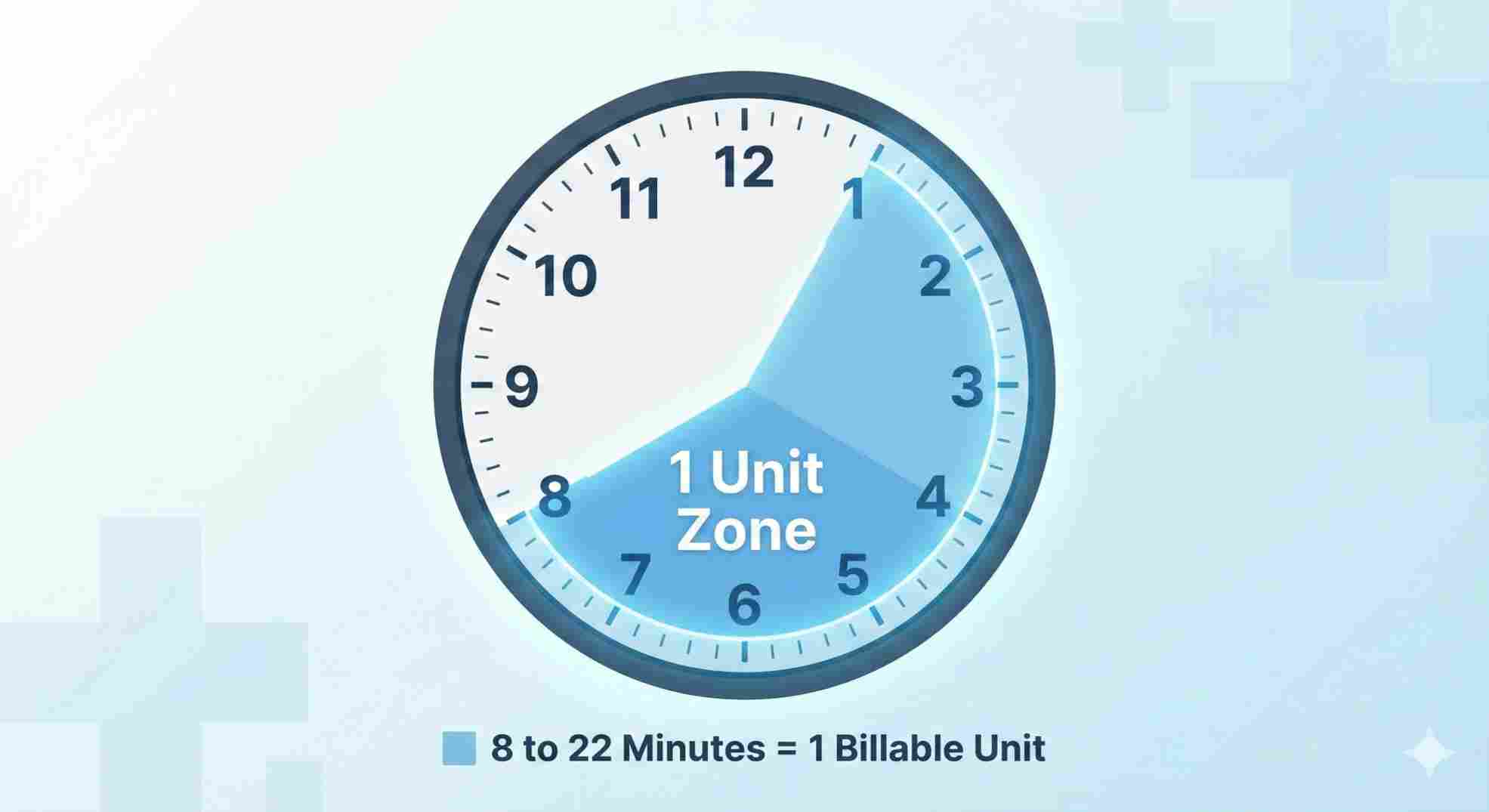
The 8-Minute Rule and Timing
Since the 97035 cpt code is time-based, you must adhere to the 8-minute rule for Medicare and most commercial payers. This rule dictates how many units you can bill based on the total time spent.
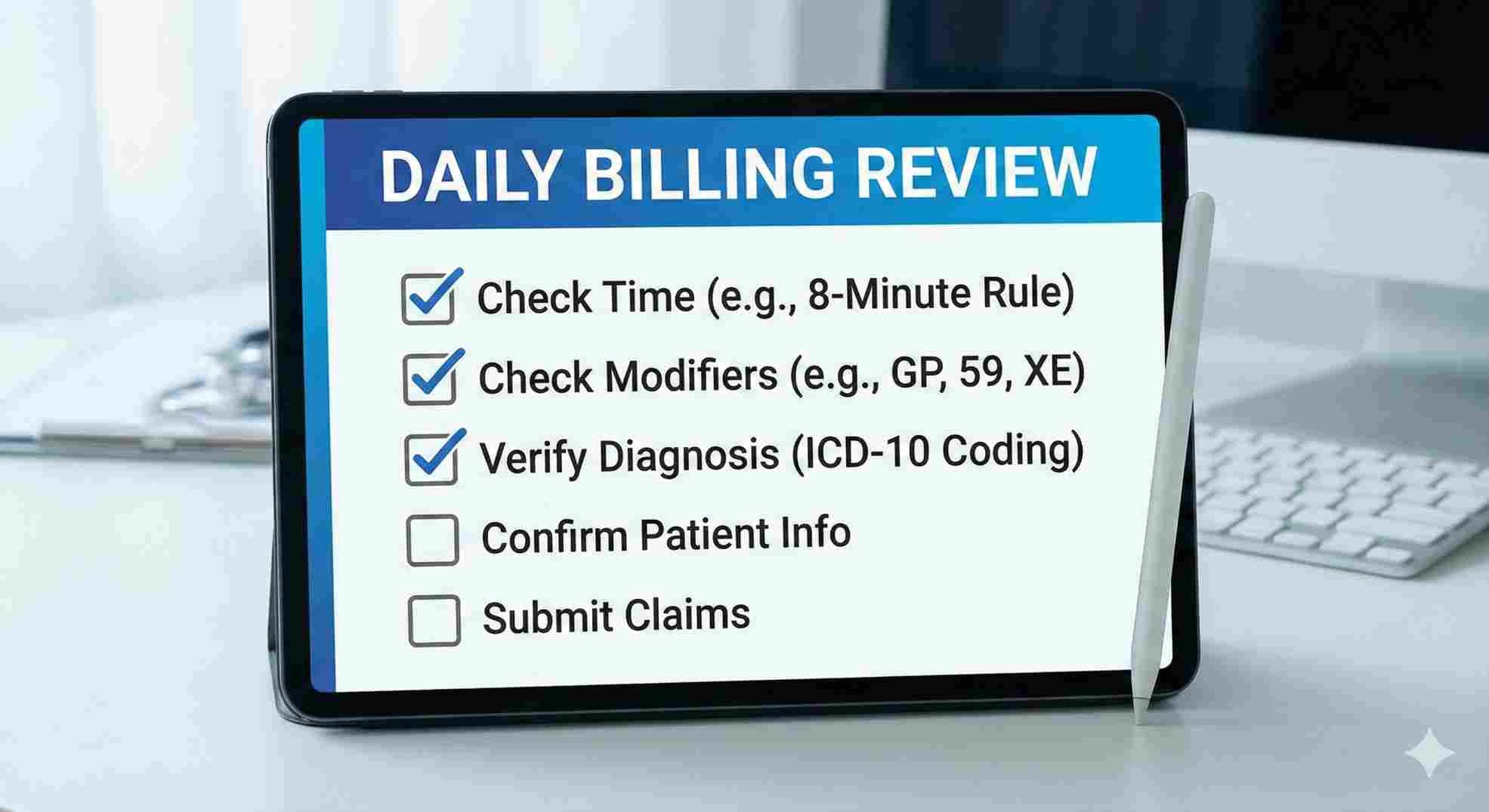
Here is a data chart to keep at your front desk.
Table 1: The 8-Minute Rule for 97035
| Total Treatment Time | Number of Billable Units |
|---|---|
| 0 minutes to 7 minutes | 0 Units (Do not bill) |
| 8 minutes to 22 minutes | 1 Unit |
| 23 minutes to 37 minutes | 2 Units |
| 38 minutes to 52 minutes | 3 Units |
| 53 minutes to 67 minutes | 4 Units |
Scenario: You apply ultrasound for 6 minutes.
Result: You cannot bill 97035 cpt code. You must count that time toward your total timed minutes for the day, but you cannot generate a specific charge for it.
Scenario: You apply ultrasound for 10 minutes.
Result: You bill 1 Unit.
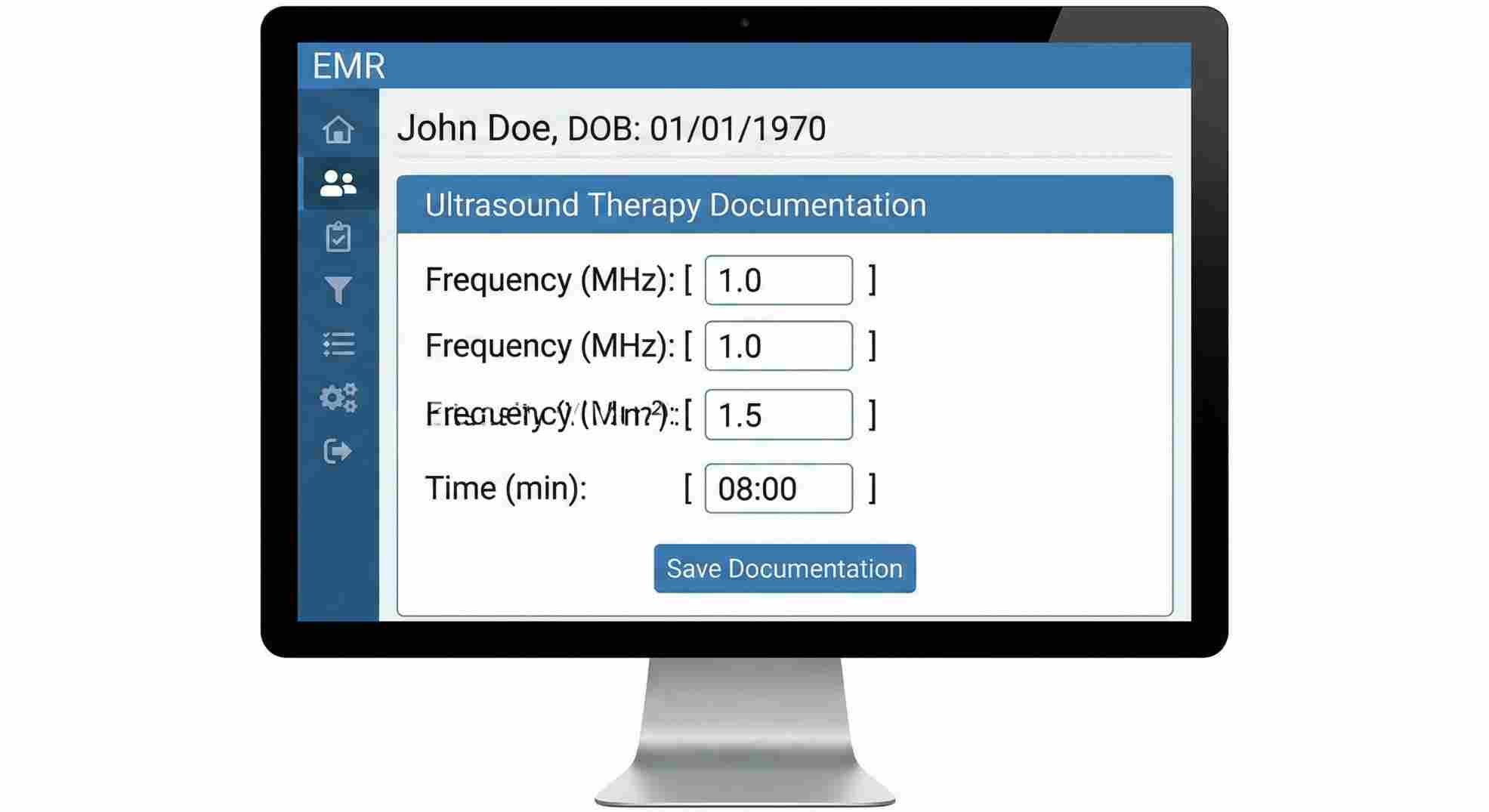
Documentation Requirements That Audit-Proof Your Practice
I have seen practices lose thousands of dollars in recoupments because their notes were lazy. When you bill the 97035 cpt code, your daily note must contain specific technical parameters.
If a reviewer looks at your note and cannot reproduce the treatment based on what you wrote, you fail the audit.
Required Documentation Elements:
- Area Treated: Be specific (e.g., “Left Lumbar Paraspinals”).
- Frequency: Usually 1 MHz (deep) or 3 MHz (superficial).
- Intensity: Watts per square centimeter (e.g., 1.5 W/cm²).
- Duty Cycle: Continuous (100% for heat) or Pulsed (20% or 50% for non-thermal).
- Duration: Exact minutes spent.
- Patient Position: (Optional but good) e.g., Prone.
Table 2: Documentation Checklist for Success
| Component | Poor Documentation Example | Audit-Proof Documentation Example |
|---|---|---|
| Specifics | Ultrasound to back. | Ultrasound to L4-L5 paraspinals, 1 MHz, 1.5 W/cm², 100% duty cycle. |
| Time | 1 unit. | 10 minutes total treatment time. |
| Rationale | For pain. | To increase tissue extensibility prior to lumbar mobilization. |
| Outcome | Patient felt better. | Post-treatment reaching increased by 10 degrees. |
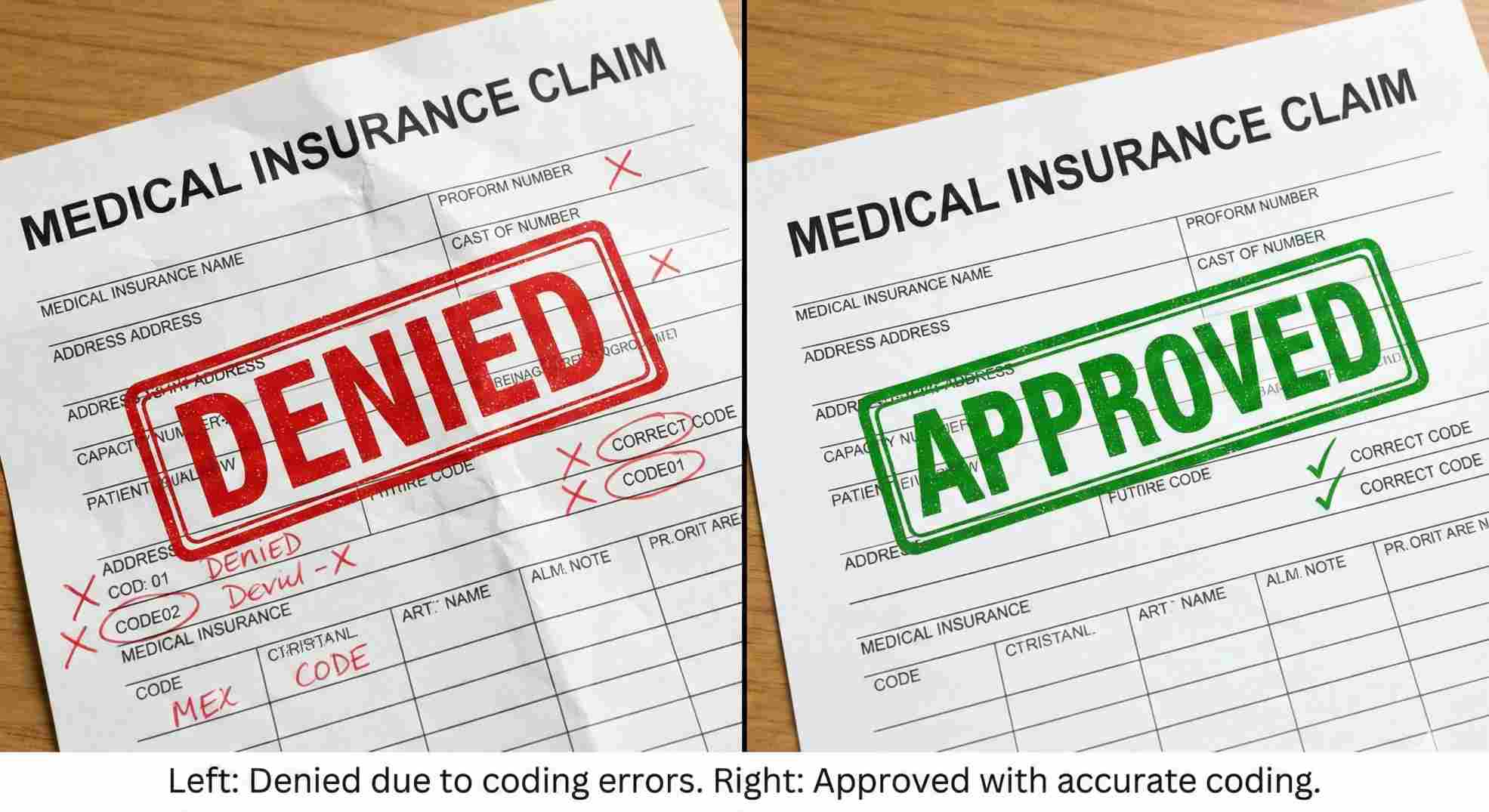
Why the 97035 CPT Code Gets Denied
Let’s get real about denials. They are the bane of our existence in healthcare. When you see a denial for the 97035 cpt code, it usually falls into one of three buckets.
1. Mutually Exclusive Procedures
This is the most common error. The National Correct Coding Initiative (NCCI) has “edits” that prevent you from billing certain pairs of codes together.
For example, if you bill a mechanical traction code and an ultrasound code for the same body part at the same time, one will get denied. The logic is that you cannot physically do both simultaneously if one requires constant attendance.
2. The “Passive Treatment” Cap
Many payers are moving toward active care models. They might pay for the ultrasound therapy cpt code for the first 6 to 12 visits. After that, they want to see the patient doing exercises (97110) or activities (97530).
If you are still billing ultrasound on visit 25 without a clear reason (like a new injury or exacerbation), expect a denial.
3. Diagnosis Mismatch
The ICD-10 code must support the treatment. If the diagnosis is “Generalized Fatigue,” ultrasound is not medically necessary. If the diagnosis is “Adhesive Capsulitis of Shoulder,” ultrasound makes perfect sense.
Reimbursement Rates: What Is It Worth?
We don’t do this just for fun; we run businesses. Reimbursement for the 97035 cpt code varies wildly based on your location and the payer.
Generally, Medicare pays less than private insurance, and Workers’ Compensation often pays the most.
National Average (Medicare):
Currently, the national average for one unit of 97035 hovers around $13 to $16.
Private Payers:
You might see rates ranging from $18 to $35 per unit.
It is not a “high dollar” code like Neuromuscular Re-education (97112), but because it is often an adjunct to other therapies, it adds up. If you treat 10 patients a day and legally bill ultrasound on 4 of them, that is an extra $60-$100 per day. Over a year, that is $25,000 in revenue. Do not ignore it, but do not rely on it as your primary income source.
Table 3: 97035 vs. Other Modalities
| CPT Code | Description | Attendance | Avg. Reimbursement |
|---|---|---|---|
| 97035 | Therapeutic Ultrasound | Constant | $13 – $18 |
| 97032 | Electrical Stimulation | Constant | $14 – $19 |
| G0283 | E-Stim (Unattended) | None | $10 – $14 |
| 97010 | Hot/Cold Packs | None | $0 (Bundled) |
Strategic Coding: Modifier 59 and Modifier GP
Sometimes you need to use modifiers to get the 97035 cpt code paid.
Modifier GP:
For Medicare patients, you must attach the GP modifier to indicate the service was provided by a physical therapist. If you miss this, the claim is rejected instantly.
Modifier 59 (or X Modifiers):
This is the “Distinct Procedural Service” modifier. You use this when you perform two services that are usually linked, but in this specific case, they were separate.
Example: You do manual therapy (97140) on the Neck, and Ultrasound (97035) on the Knee.
Normally, these might flag an edit. By adding Modifier 59 (or XS for Separate Structure) to the 97035 cpt code, you tell the payer, “Hey, I know these usually go together, but I treated a totally different body part.”
Use this carefully. Overusing Modifier 59 is a fast track to an audit.
Conclusion: Master the 97035 CPT Code
Billing isn’t the most exciting part of healthcare, but it is the fuel that keeps your clinic running. The 97035 cpt code is a staple in physical therapy, chiropractic, and rehabilitation clinics. It represents a valuable service that helps patients recover from pain and inflammation.
Don’t let fear of audits stop you from billing for the work you do. Documentation is your shield. If you time your treatments correctly (respecting the 8-minute rule), document the specific settings (MHz, Intensity), and ensure the diagnosis supports the need for deep heat, you will secure your revenue.
Take a look at your last month of claims. Did you bill the 97035 cpt code correctly? If not, use this guide to fix your process tomorrow. Your practice—and your patients—will be better for it.
FAQs About 97035 CPT Code
Can I bill 97035 if I use a hands-free ultrasound device?
How many units of 97035 can I bill in one session?
Is the 97035 cpt code description the same for phonophoresis?
Can I bill 97035 and 97140 (Manual Therapy) together?
Does Medicare cover 97035?
Schedule Zoom Meeting
Let’s face it: you didn’t enter the field of behavioral health to spend your evenings fighting with insurance adjusters over denied claims. But the reality is, mental health billing is notoriously messy, and without a specialized strategy, you are likely leaving 15-20% of your revenue uncollected. Stop letting complex coding requirements and payer loopholes dictate your facility’s financial health. You need a partner who understands the specific nuances of your specialty—from crisis intervention to time-based therapy codes—so you can focus entirely on patient care. Ready to stop the revenue leaks? Contact us today for a complimentary practice audit, and let’s ensure you get paid for every minute of the incredible work you do.

