How to Bill Insurance for Therapy: Updated Guide 2026
Table of Contents
Learning how to bill insurance for therapy is rarely part of the grad school curriculum. You went to school to decipher complex trauma and help broken families, not to fight with UnitedHealthcare over a rejected claim.
But here is the cold reality of private practice: You can be the best clinician in the world and still go broke.
There’s a weird myth in our field that billing is just “admin work”—something annoying you do on Friday afternoons. That mindset is dangerous. The therapists who actually stay in business understand that insurance billing isn’t paperwork. It’s the lifeblood of your practice.
Most courses won’t tell you this, but 90% of claim denials have nothing to do with the therapy session itself. They happen before the client even walks through your door.
If you are waiting until you sit down with a CMS-1500 form to figure out if you’re getting paid, you have already lost.
The Golden Rule: Trust No One
The secret to getting paid isn’t memorizing a thousand codes. It comes down to one harsh rule: Never trust what the client tells you about their coverage.
Your client isn’t lying. They just don’t know. They don’t know the difference between a PPO and an HMO. They don’t know that their deductible resets in January, or that their plan covers “mental health” but carves out “behavioral health” to some random third-party payer you’ve never heard of.
If you want to survive, you have to treat billing as a clinical boundary. You check the benefits yourself, every single time, before the first session.
Key Takeaways
- Call Them: Checking benefits (VOB) personally is the only safety net you have.
- Watch the Clock: CPT codes are strict about time. If you bill a 60-minute code for a 45-minute session, you are asking for an audit.
- It’s About Illness: Insurance pays for the treatment of a medical condition, not “personal growth.” Your notes have to prove that.
- 90 Days or Bust: Most insurers have a “timely filing” window. If you submit on day 91, you just worked for free.
Phase 1: The Setup (Before You Bill a Cent)
You can’t bill if you don’t exist in their system. Before you see a single insurance client, you need three specific identifiers.
- NPI (National Provider Identifier): This is your HIPAA ID card. You can register for your Type 1 (Individual) NPI directly through the NPPES registry. If you set up an LLC, you’ll also need a Type 2 (Group) NPI.
- Tax ID (EIN): Do not use your Social Security Number on claim forms. It’s a massive security risk. Get an EIN from the IRS. It’s free and takes five minutes.
- CAQH ProView: Think of CAQH as a universal filing cabinet. You upload your resume, license, and liability insurance here once, and the insurance companies pull your data from it. Heads up: You have to log in and click “Re-attest” every 120 days, or insurers will drop you.
Credentialing vs. Contracting
Credentialing is just the insurer checking your background. Contracting is the money part.
- In-Network (Paneling): You sign a contract accepting their rate (say, $105 per session). You cannot ask the client to pay the difference between your normal rate and the insurance rate. That’s illegal “balance billing.”
- Out-of-Network (OON): No contract. You charge your full fee, and the client tries to get paid back using a Superbill you provide.
Phase 2: The Rosetta Stone of CPT Codes
Mental health billing runs on CPT codes. If you use the wrong one, the computer system kicks it back automatically.
The big change for 2026: Time requirements are strict. According to the American Medical Association, you must document the actual face-to-face time spent with the patient to justify the code.
Essential Therapy CPT Codes & Time Rules
| CPT Code | Description | Time Required | Best Used For… |
|---|---|---|---|
| 90791 | Psychiatric Diagnostic Evaluation | N/A (Untimed) | The Intake. You usually only bill this once per client. |
| 90834 | Psychotherapy, 45 minutes | 38–52 minutes | The standard session. This is the safest code to use to avoid audits. |
| 90837 | Psychotherapy, 60 minutes | 53+ minutes | Long sessions. Warning: Insurance companies hate this code. Use it sparingly. |
| 90847 | Family/Couples Therapy | 26+ minutes | Therapy with the client present (Partner/Parent). |
| 90846 | Family Therapy (w/o Client) | 26+ minutes | Talking to parents or partners without the patient in the room. |
| +90839 | Crisis Psychotherapy | First 60 mins | Urgent, high-risk situations. Your notes need to be perfect for this. |
The Telehealth Trap
Since 2020, billing for video sessions is normal, but the coding is tricky.
- Place of Service (POS): You usually use 02 or 10 depending on if the client is at home.
- Modifiers: You often have to add 95 or GT to the code (like
90837-95) to show it was video. If you forget this little tag, the claim gets denied.
Phase 3: The Claim (Mastering the CMS-1500)
The CMS-1500 is the standard red-ink form maintained by the National Uniform Claim Committee. Whether you use software like SimplePractice or type it out manually, the data fields are the same.
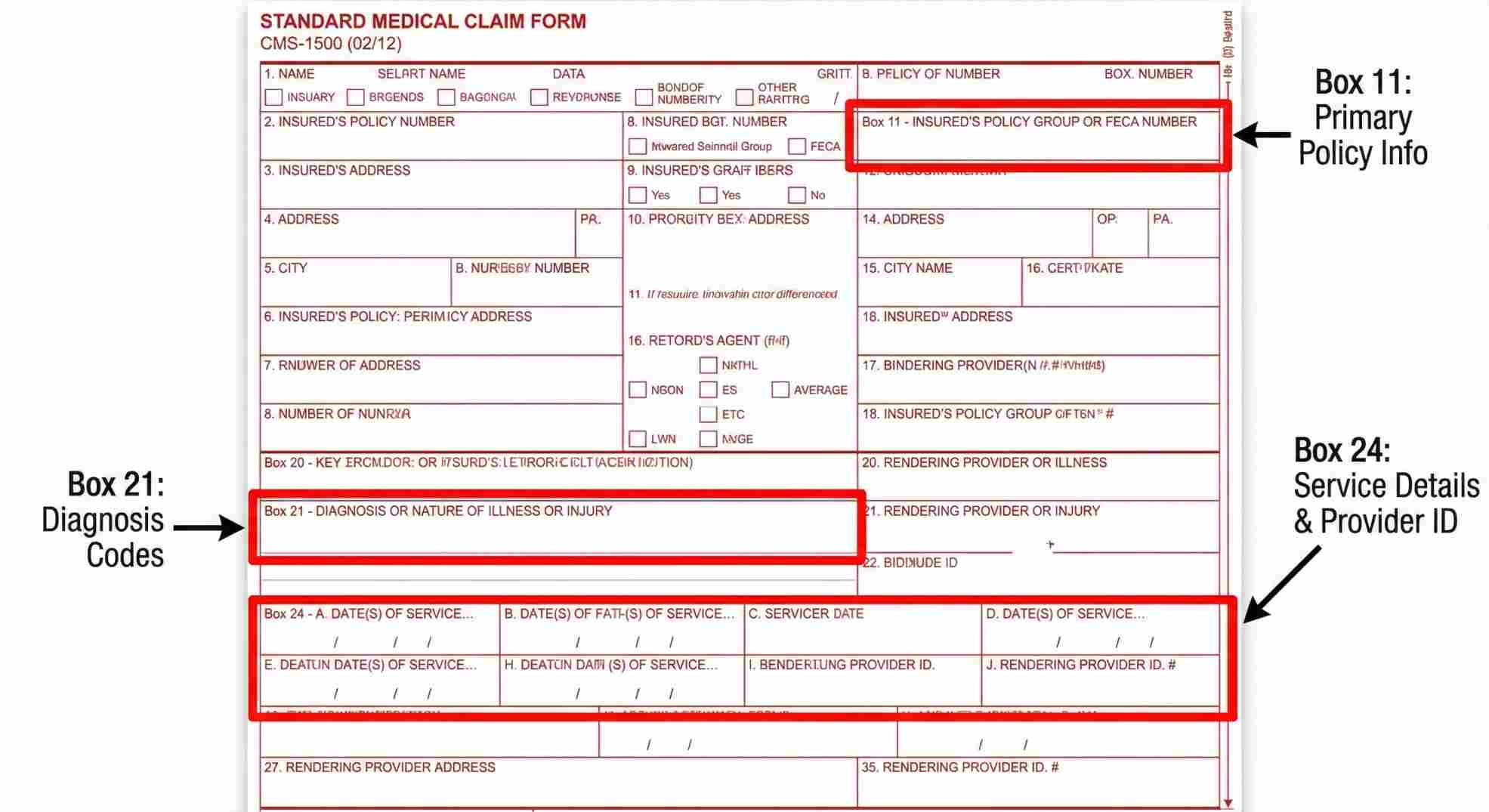
Where Everyone Messes Up
Three specific boxes cause almost all rejections:
- Box 11 (Insurance Policy Group): This connects the patient to the main policyholder. If you are treating a child, the “Insured” is the parent, not the kid. If you spell the name “Ben” instead of “Benjamin,” the computer rejects it.
- Box 21 (Diagnosis): You must use ICD-10 codes (like F41.1 for Anxiety). Stay away from Z-codes as the primary diagnosis. Insurance pays for medical necessity. A “relationship problem” (Z-code) isn’t a medical illness in their eyes.
- Box 24J (Rendering Provider): If you are in a group practice, this box needs your personal NPI. Box 33 gets the Group’s NPI. Mix these up, and the check goes to the wrong place—or nowhere at all.
Phase 4: Medical Necessity & The “Golden Thread”
If you get audited, the auditor is looking for one thing: the Golden Thread.
This is the logical line that connects your paperwork:
Diagnosis → Treatment Plan → Progress Note
If you bill a 90837 (60 minutes) for Major Depressive Disorder, your note cannot just say, “Client talked about work stress.” That looks like paid friendship, not healthcare.
Your note needs to say something like:
“Used CBT techniques to identify cognitive distortions regarding workplace performance, directly addressing depressive symptoms of worthlessness. Client practiced reframing negative self-talk.”
Pro Tip for Couples Counselors: Insurance does not cover “marriage counseling.” It covers treating one person’s mental health issue with the partner present. The focus always has to be on the medical condition of the identified patient.
Phase 5: Troubleshooting & Rejections
You sent the claim. You waited a month. You got $0.
Welcome to the EOB (Explanation of Benefits). This is the letter telling you why they didn’t pay.
Top Denial Reasons & How to Fix Them
| Denial Code | Translation | The Fix |
|---|---|---|
| CO-4 | “Code inconsistent with modifier.” | You probably billed a video session but forgot the -95 modifier. Add it and resubmit. |
| CO-11 | “Diagnosis code inconsistency.” | You used a diagnosis they don’t cover (like a Z-code). You need a valid F-code. |
| CO-27 | “Coverage terminated.” | The client lost their job or switched plans. You are likely out of luck. This is why you verify benefits first. |
| CO-29 | “Time limit expired.” | You waited too long to file (usually 90 days). You can try to appeal, but you’ll probably have to write off the loss. |
| PR-1 | “Deductible Amount.” | The insurance approved the claim, but they aren’t paying. The client owes you this money. |
Conclusion: The Business of Healing
Learning how to bill insurance for therapy isn’t just about cash flow; it’s about access. By figuring this stuff out, you let clients get care they couldn’t afford otherwise.
But remember: You run a business.
- Verify benefits before the session.
- Write notes for medical necessity, not just a diary entry.
- Check your Aging Report once a month to catch unpaid claims.
Don’t let the paperwork burn you out. Master the system so you can get back to what actually matters: the person sitting in the chair across from you.
FAQs About How to Bill Insurance for Therapy
Can an intern or non-licensed therapist bill insurance?
What is the difference between a co-pay and coinsurance?
Can I bill for two sessions in one day?
What is a "Recoupment" or "Clawback"?
Should I just hire a billing service?
Schedule Zoom Meeting
If you are tired of chasing denials and spending hours on hold with insurance companies, it might be time to bring in the experts. You deserve to focus on your clients, not on fighting for every dollar. Stop letting administrative headaches drain your energy and your revenue. We can help you streamline your practice, reduce rejections, and finally get paid what you earn.

