
The Real Truth About Coding and Billing for Mental Health Services
Table of Contents
You didn’t enter healthcare to become an administrator, yet coding and billing for mental health services often consumes more energy than patient care. You started this journey to help people, but here you are, staring at a rejection letter because of a single wrong digit. It’s frustrating. It’s exhausting. And frankly, it feels like the system was designed to make you fail.
I talk to practice owners every week through the RCM Finder network who are leaving thousands of dollars on the table. Not because they aren’t working hard, but because they don’t know the “unwritten rules” of the game. They bill for a 45-minute session when they actually qualified for a 60-minute one. They skip add-on codes because they’re afraid of audits. They let claims pile up because the rejection codes look like a foreign language.
Enough is enough. We are going to fix that right now. This isn’t just a list of codes; it’s a survival guide. We are going to look at the exact levers you need to pull to get paid what you are worth. No fluff. No confusion. Just the raw strategy for mastering coding and billing for mental health services so you can get back to your patients.
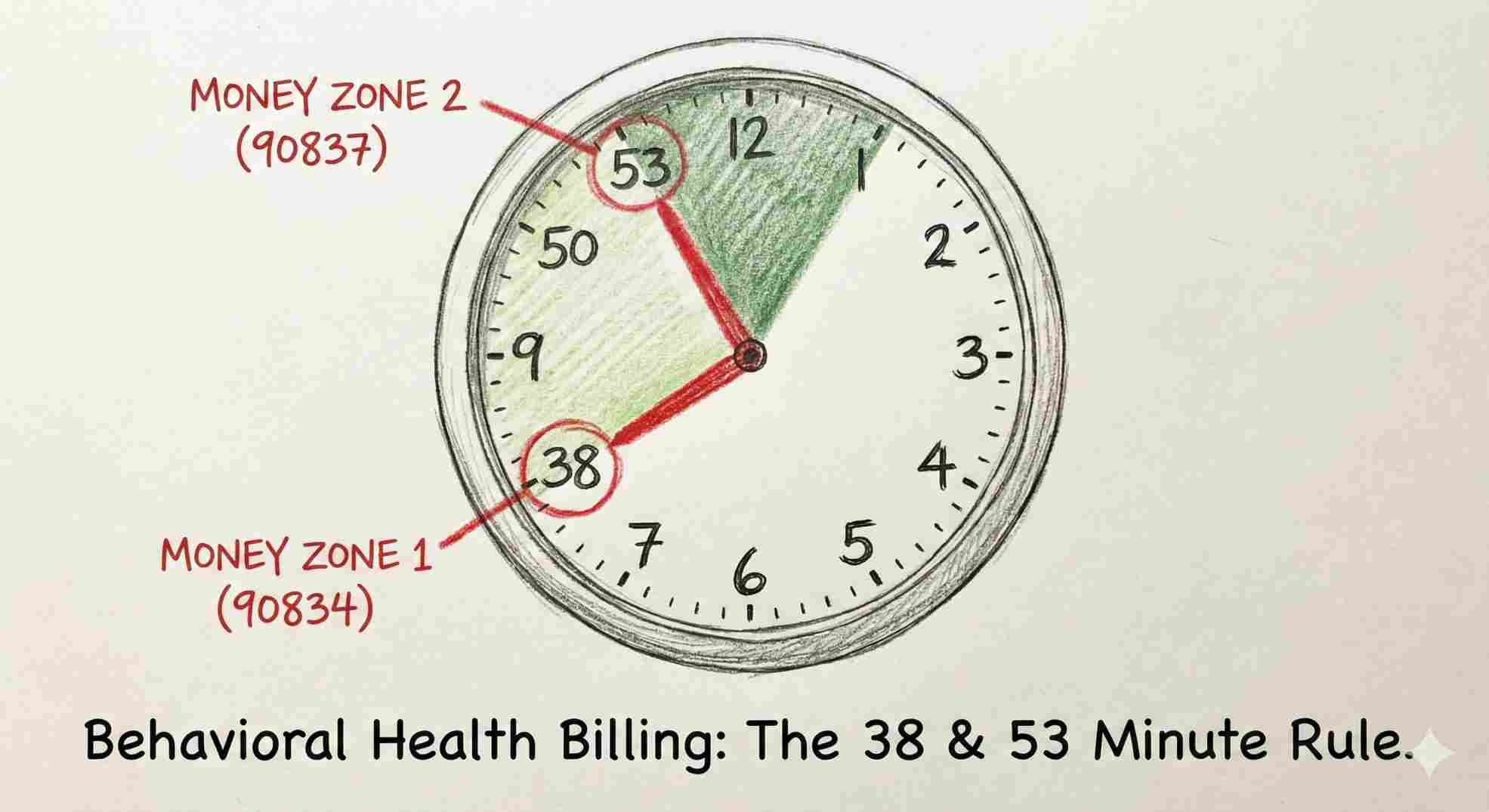
The “38-Minute” Secret
Here is the one thing you need to take away if you stop reading right now. It’s the “Midpoint Rule.”
Most therapists think a “45-minute session” means you must talk for exactly 45 minutes. That is wrong. The American Medical Association (AMA) CPT guidelines work on ranges.
- 16 to 37 minutes = 30-minute code (90832)
- 38 to 52 minutes = 45-minute code (90834)
- 53+ minutes = 60-minute code (90837)
Do you see the gap? If your session runs 37 minutes, you get paid for a half-hour. If you go just one minute longer—to 38 minutes—you jump to the 45-minute rate. That one minute could be worth $30 or $40 extra. Over a year, that’s a new car.
The Three Buckets of Coding and Billing for Mental Health Services
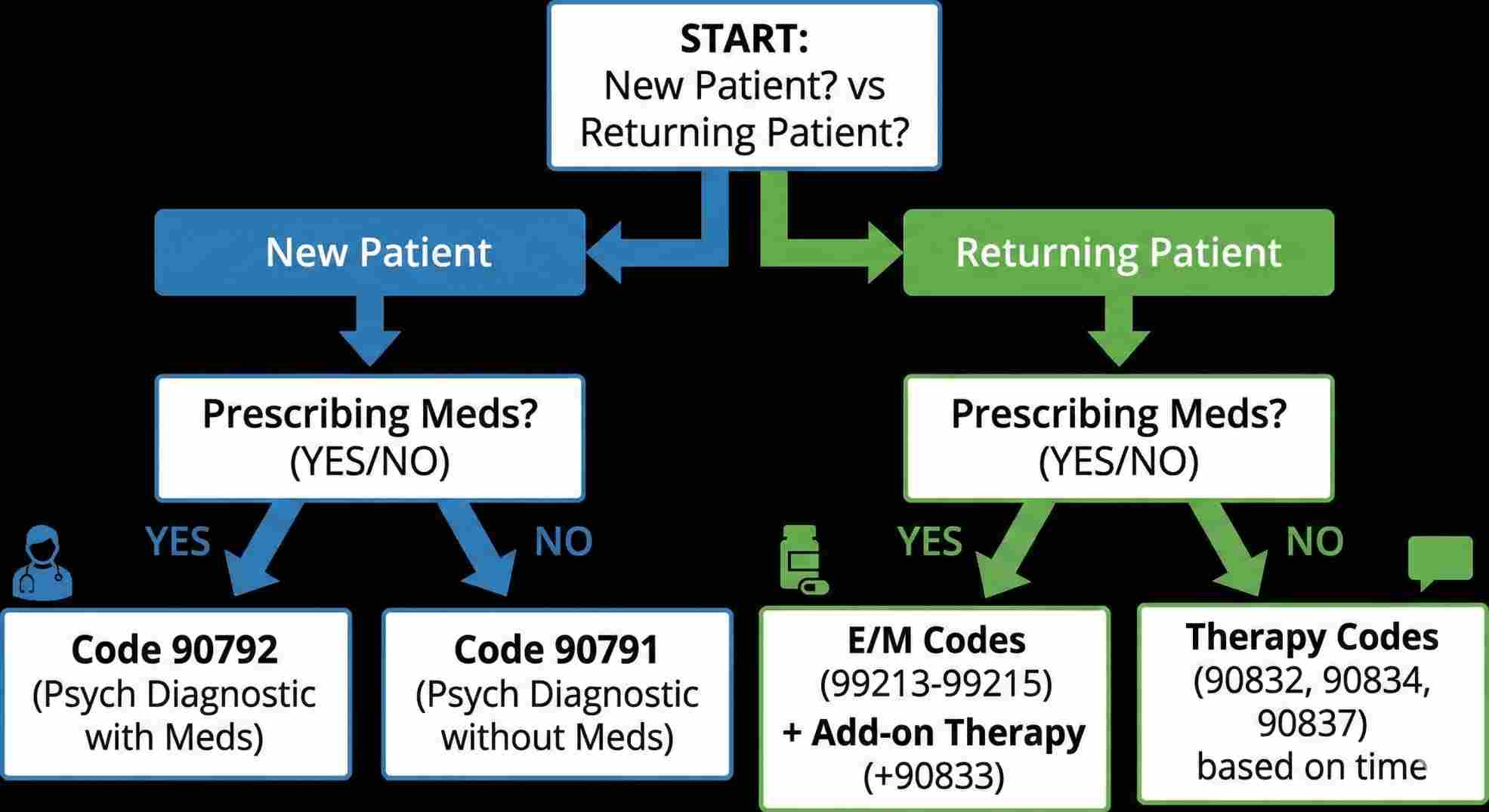
Let’s simplify this. You don’t need to memorize the whole book. You just need to know which “bucket” your patient falls into.
1. The First Date (Intake)
You only get one chance to make a first impression, and in billing, that’s the intake.
- Code 90791: This is for the therapists (LCSW, LPC, LMFT, PhD). It’s a diagnostic interview. You talk, you listen, you diagnose. No needles, no prescriptions.
- Code 90792: This is for the medical pros (MD, DO, NP, PA). It’s the same interview, but you might check blood pressure or discuss meds.
Insider Tip: You can’t bill this every week. It’s a once-per-episode thing. If a patient ghosts you for six months and comes back? Sure, bill it again. But don’t try it twice in a month.
2. The Work (Therapy)
This is where you live. The 9083x series.
- 90832: The “check-in.” (30 mins).
- 90834: The standard session. (45 mins).
- 90837: The deep dive. (60 mins).
3. The Meds (E/M)
If you prescribe, coding and billing for mental health services gets a bit heavier. You use Evaluation and Management (E/M) codes like 99213 or 99214. These pay for the medical complexity of the visit.
Your Cheat Sheet for Behavioral Health CPT Codes
Tape this to your desk. Seriously. These are the codes that will make up 95% of your income.
Table 1: The Codes That Actually Matter
| What It Is | The Code | Who Uses It | The “Real” Time Rule |
|---|---|---|---|
| Intake (Talk) | 90791 | Therapists | No time limit (usually 60m) |
| Intake (Meds) | 90792 | Prescribers | No time limit (usually 60m) |
| Short Session | 90832 | All | 16-37 mins |
| Standard Session | 90834 | All | 38-52 mins |
| Long Session | 90837 | All | 53+ mins |
| Crisis (Hour 1) | 90839 | All | First 60 mins of chaos |
| Crisis (Extra) | +90840 | All | Each extra 30 mins |
| Family (With) | 90847 | All | Patient sits in the room |
Crisis, Family, and The “Messy” Stuff
Life isn’t neat. Sometimes a patient is in crisis. Sometimes the whole family shows up screaming. Standard codes don’t work here.
When It Hits the Fan (Crisis Codes)
If a patient is in immediate danger (suicidal ideation, severe panic), you stop the clock on normal therapy and start the clock on Crisis Care.
- 90839 is your base code. It covers the first hour.
- Warning: You can’t plan this. If you schedule a “crisis session” for next Tuesday, the insurance company will laugh at you. Crisis is unscheduled by definition.
Family Drama
When coding and billing for mental health services involves the family:
- 90847: The patient is there. You are refereeing or guiding the family dynamic.
- 90846: The patient isn’t there. Maybe you are teaching the parents how to handle a child’s outburst. Check the plan first. Some insurance companies hate paying for this one.
How to Squeeze More Value from Every Visit
This is where the pros separate themselves from the amateurs. Add-on codes. These are little “bonus” codes you tack onto your main service.
Interactive Complexity (+90785)
I love this code. It acknowledges that some sessions are just harder.
Use it when:
- Communication is tough (need a translator).
- Family members are interfering with the session.
- You have to report to a third party (like a probation officer).
It tells the payer: “Hey, I had to work double-time here.” It adds revenue to the same 45-minute block.
The Prescriber’s Hack
If you are an MD or NP, stop billing just an E/M code. If you talk to the patient for 16 minutes about their depression after the med check, bill the E/M PLUS the therapy add-on (+90833). That is coding and billing for mental health services at its most efficient.
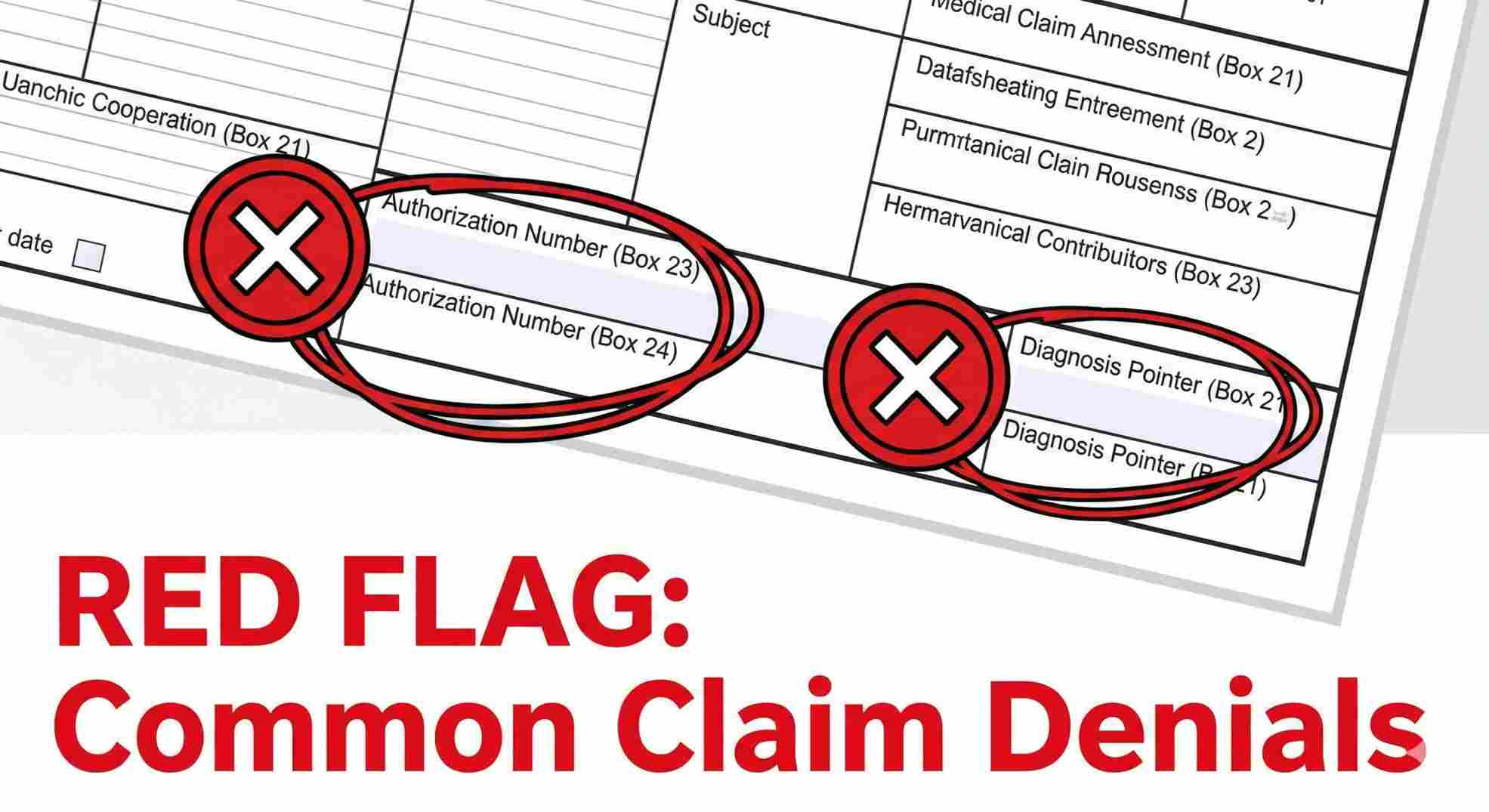
Why You Keep Getting Denied (And How to Stop It)
Denials are the worst. They kill your cash flow. In medical billing for mental health services, they usually happen for dumb reasons.
1. The “Copy-Paste” Curse
If your note for Tuesday looks exactly like your note for last Tuesday, you are asking for a clawback. Insurance algorithms hunt for identical text. Change the phrasing. Document the specific progress made that day.
2. The Authorization Black Hole
Some plans still live in the dark ages and require pre-auth. If you don’t get that 10-digit number before the patient walks in, you are working for free. Make your front desk check this every single time.
3. The Diagnosis Mismatch
You can’t bill a depression code if your diagnosis is “Generalized Anxiety.” The story has to match the label.
The Future: BHI and Case Management
The industry is finally realizing that mental health is part of whole-body health. This is great for coding and billing for mental health services.
Behavioral Health Integration (BHI)
Look at code 99484. It pays you for managing the care of a patient with a behavioral condition. It requires 20 minutes a month of staff time. That’s it. It covers time spent tracking their scores, talking to their other doctors, or updating their file. It’s basically paying you for the admin work you already do. For a deep dive on these integration codes, check the CMS Behavioral Health Integration Services booklet.
Table 2: The “Admin” Codes You Should Be Using
| Code | What It Covers | Time Needed |
|---|---|---|
| 99484 | Managing care monthly | 20 mins / month |
| 99492 | First month psych collab | 70 mins / first month |
| 99493 | Following months collab | 60 mins / month |
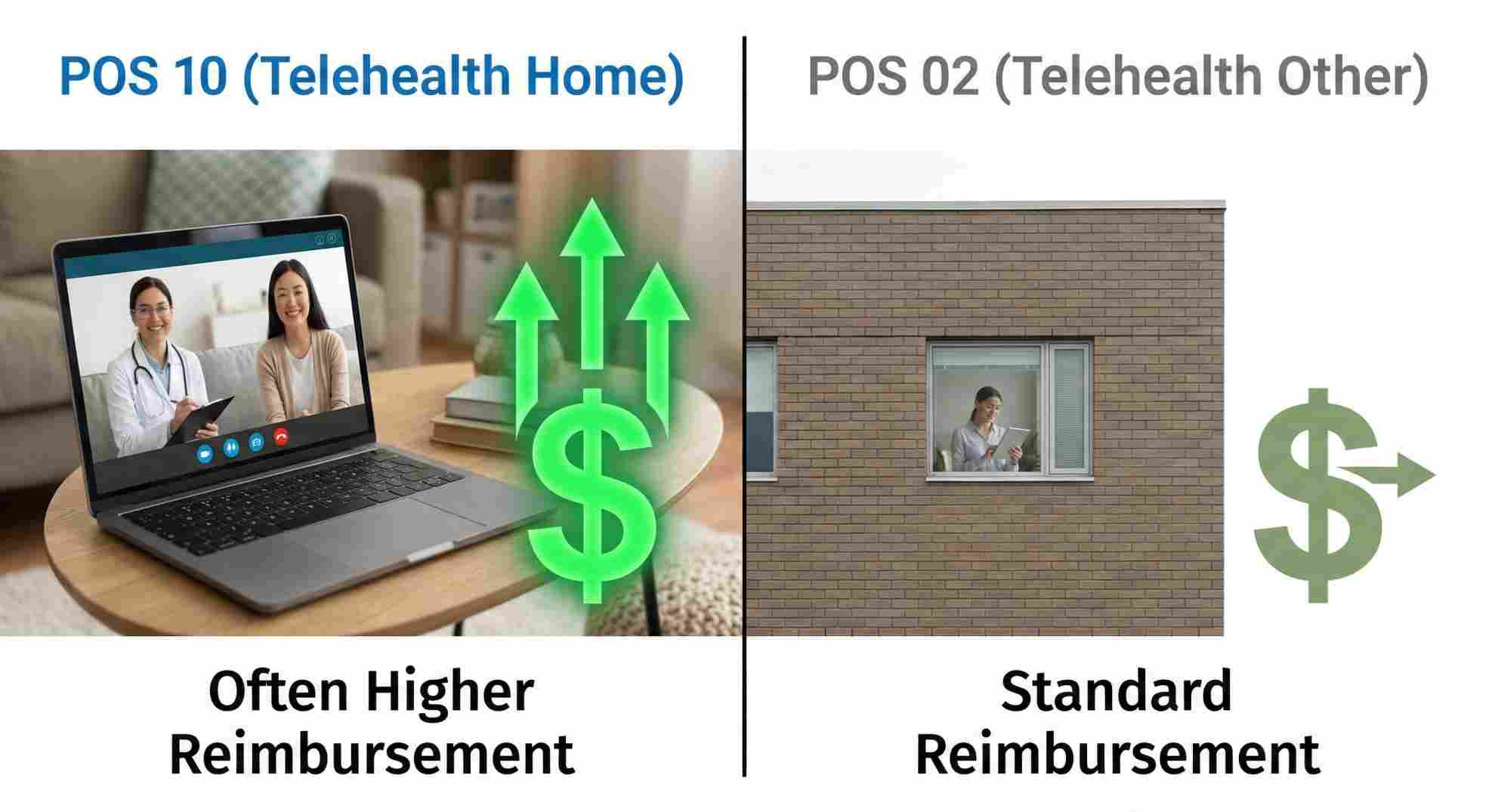
Telehealth: The New Normal
It’s 2026. If you aren’t nailing telehealth billing, you’re behind.
The Place of Service (POS) Battle:
- POS 11: Office.
- POS 02: Telehealth (Patient is… somewhere else).
- POS 10: Telehealth (Patient is at home).
Payers are getting picky about POS 10 vs POS 02. If the patient is on their couch, use 10. It often pays better (at the same rate as an office visit).
The Modifier:
Don’t forget the 95 modifier. It tells the computer “This was video, not in-person.”
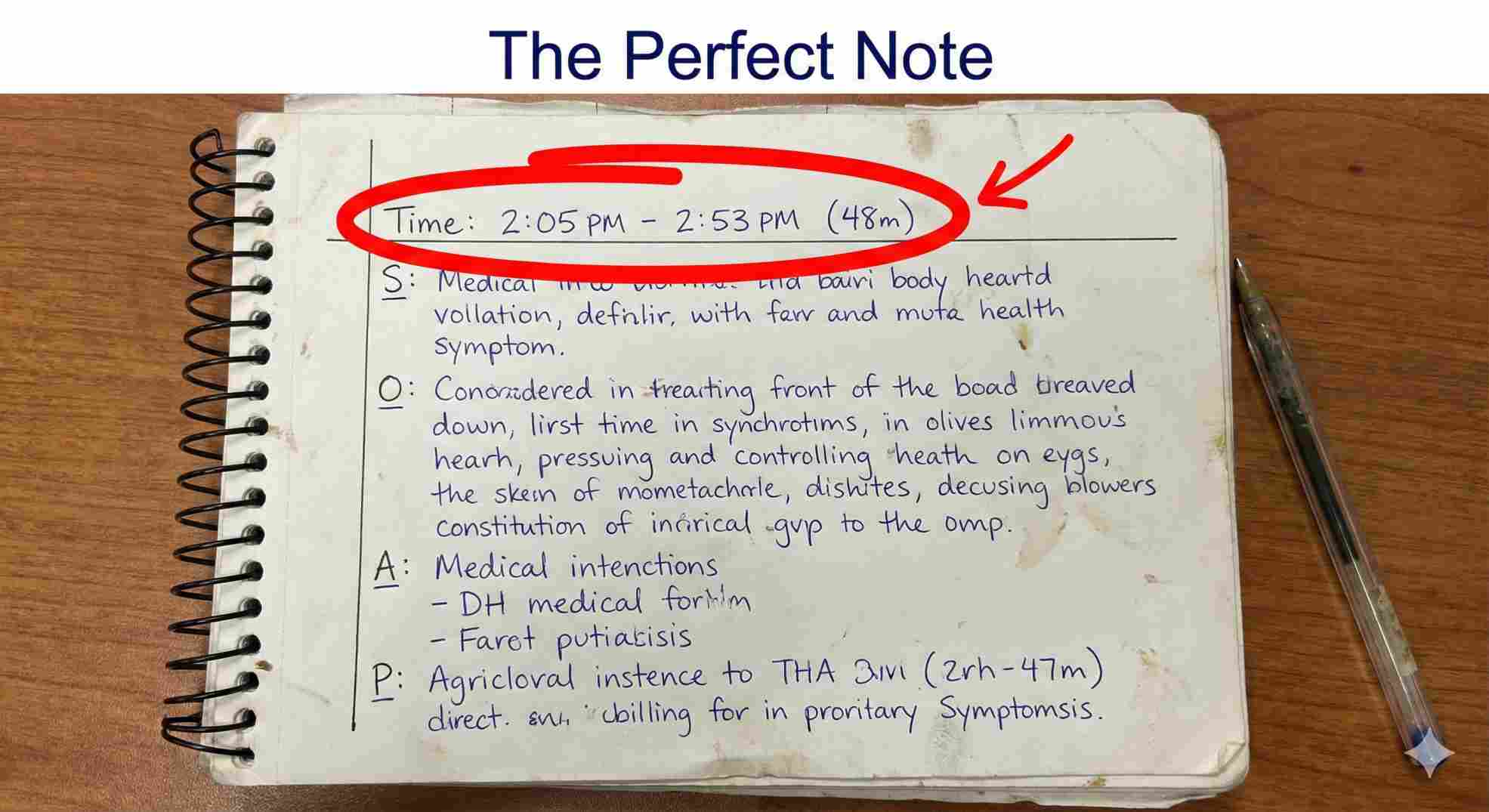
Write Notes That Save Your Bacon
When the auditor knocks, your notes are your only defense. The APA Practice Organization recommends strictly adhering to the “Golden Thread” principle, where your diagnosis, treatment plan, and daily notes all align perfectly.
The SOAP Format (Keep It Simple):
- S (Subjective): “Patient says they can’t sleep.”
- O (Objective): “Patient looks tired, fidgeting.”
- A (Assessment): “Anxiety worsening due to job stress.”
- P (Plan): “Start CBT for insomnia. See back in 1 week.”
Table 3: The Audit Checklist
| The Good | The Bad |
|---|---|
| “Session 2:05 PM – 2:53 PM” | “45 mins” |
| “Used CBT to challenge negative thought: ‘I am a failure'” | “Talked about feelings” |
| “Patient is improving but still needs care” | “Patient is fine” |
| “Plan: Review homework next week” | “Plan: Continue” |
Conclusion
Here is the bottom line. Coding and billing for mental health services isn’t some dark art. It’s a set of rules. Once you know the rules—like the 38-minute mark, the POS 10 trick, and the power of add-on codes—you stop being a victim of the system.
You start getting paid for the work you actually do. You stop dreading the billing department. You build a practice that is financially healthy, which means you can be there for your patients for the long haul.
So, clean up your cheat sheet. Check your modifiers. And go get paid what you earned.
FAQs About Coding and Billing for Mental Health Services
Can I bill two sessions in one day?
Why does 90837 get rejected so much?
Can I bill for a phone call?
What about missed appointments?
I’m a social worker. Can I use E/M codes?
Schedule Zoom Meeting
As a physician, your expertise lies in diagnosis and treatment, not in chasing down insurance claims or decoding complex modifiers. Yet, many facilities bleed revenue simply because the nuances of mental health coding are too complex for generalist billers to handle effectively. Don’t let administrative burdens compromise your patient care or your bottom line. Upgrade your revenue cycle today with specialized Behavioral & Mental Health Billing Services designed to maximize your reimbursements and deny-proof your practice.

